Scientific Calendar March 2018
Which platelet-related indications would typically be seen on a haematology analyser during early response to severe viraemia?
Thrombocytopenia and increased IPF
Thrombocytosis and increased IPF
Thrombocytosis and low IPF
Thrombocytopenia and low IPF
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background information
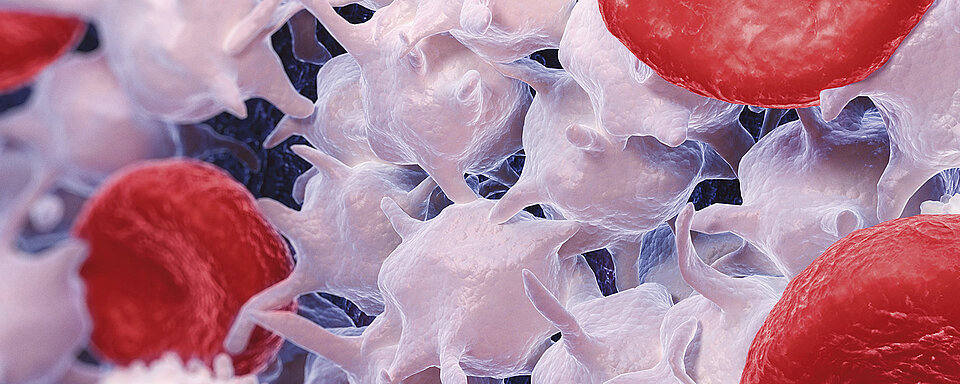
Platelets are traditionally recognized for their key role in haemostasis, for example sealing vessel breaches and limiting blood loss. However, in recent years, it has become evident that platelets also have potential as immune modulators and effectors with various inflammatory functions (1).
Systemic viral infections such as hepatitis C or HIV are often associated with thrombocytopenia. Rapidly induced thrombocytopenia in response to viral infection is mediated via increased platelet destruction, whereas thrombocytopenia induced by decreased platelet production is observed at later stages of infection.
Several host-protective mechanisms resulting in virus-induced thrombocytopenia have been proposed to cause fast platelet destruction during early stages of infection (2). Viruses can directly interact with platelets, or platelets can recognize immunocomplexes of immunoglobulins and viral antigens. Viral antigens often show cross-reactivity with platelet surface integrins, which provides another mechanism of virus-induced thrombocytopenia. The virus-induced pro-inflammatory cytokines often lead to platelet activation and destruction in viraemic patients. All these mechanisms lead to increased platelet clearance from the blood. The activated platelets are recognized by circulating leucocytes or by cells in the spleen and liver and rapidly cleared from the circulation (2).
During later stages of infection, viruses can modulate platelet production at various steps of development. They are able to influence the cytokine profile of the host, resulting in altered thrombopoietin (TPO) production in the liver. The hepatitis C virus also directly interferes with TPO production by destroying liver tissue. Furthermore, viruses can influence platelet production via the induction of interferons, which suppress platelet formation and lead to thrombocytopenia. Other mechanisms involve the infection of megakaryocytes or haematopoietic stem cells (2).
Due to the mechanisms of increased platelet destruction in peripheral blood during very early response to viral infection, the low PLT count is often associated with an increased immature platelet fraction (IPF), which reflects the effort of compensating for platelet loss by producing new immature platelets. Later stages of virus-induced thrombocytopenia with decreased bone marrow platelet production would be indicated by low IPF values, reflecting the insufficient megakaryocytic production and release of new platelets into peripheral blood.
Virus-induced thrombocytopenia
Decreased platelet production | Increased platelet destruction |
|---|---|
| Infection of megakaryocytes | Direct interaction of virus with platelet |
| Infection of haematopoietic stem cells | Platelet interaction with immunocomplexes of immunoglobulins and viral antigens |
| Increased levels of interferons | Binding of virus-induced antiplatelet antibodies |
| Decreased thrombopoietin production | Virus-induced pro-inflammatory environment |
| Changes in the portal vein pressure | |
| Sequestration in the enlarged spleen |
Table 1 Mechanisms of virus-induced thrombocytopenia, either via decreased platelet production or increased platelet destruction (2).
References
1. Jenne CN et al. (2015): Platelets in inflammation and infection. Platelets. 26(4):286-92.
2. Assinger A (2014): Platelets and infection – an emerging role of platelets in viral infection. Front Immunol. Dec 18; 5:649.