Scientific calendar February 2022
Treatment of acquired TTP with caplacizumab
Which laboratory parameters are affected by caplacizumab and how?
VWF activity and antigen are increased, while FVIII:C level is decreased.
FVIII:C, VWF activity and antigen levels are increased.
FVIII:C, VWF activity and antigen levels are decreased.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
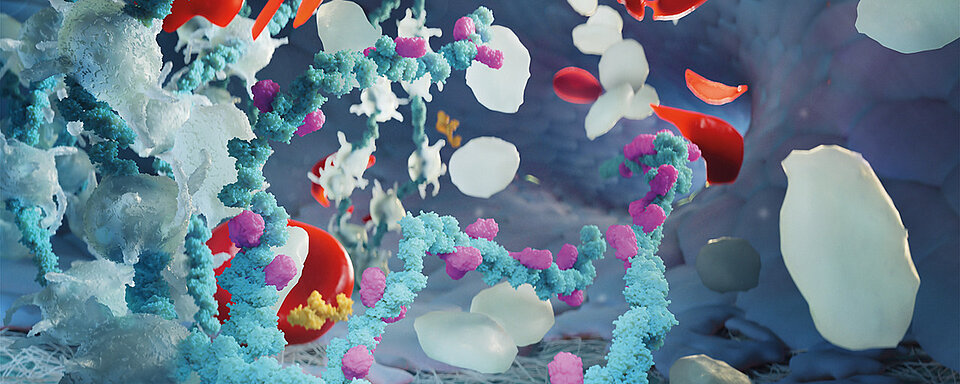
Caplacizumab (Cablivi®, Sanofi-Aventis) is a humanised, bivalent nanobody targeting the A1 domain of von Willebrand factor (VWF) used for the treatment of acquired thrombotic thrombocytopenic purpura (aTTP) in combination with plasmapheresis and immunosuppression (1, 2). aTTP is a rare, life-threatening autoimmune blood clotting disorder caused by inhibitory autoantibodies to the von Willebrand factor (VWF)-cleaving protease ADAMTS-13. Decreased ADAMTS-13 activity leads to accumulation of extremely large (UL) VWF multimers, which bind to platelets and induce microthrombus formation, cause tissue ischaemia and organ dysfunction, and potentially lead to overt severe thromboembolic complications such as stroke and myocardial infarction, and arterial and venous thrombosis (3, 4, 5, 6).
The pharmacological action of caplacizumab results in a reduction of VWF activity (ristocetin-induced platelet aggregation (RIPA) or ristocetin cofactor (VWF:RCo)) and VWF antigen levels (VWF AG). Since coagulation factor VIII (FVIII) is bound in a complex to VWF in the blood, a reduction in the coagulation factor VIII concentration (FVIII:C) in plasma occurs in parallel (7). Patients under stable therapy with a daily subcutaneous dose of 10 mg caplacizumab have a VWF AG level reduced by approx. 50% with a similarly strong reduction in FVIII:C (7). The reduction of the VWF activity is markedly greater than that of the antigen level: VWF:RCo falls below 20% and RIPA below 10% of the norm (7). However, the reduced VWF and FVIII:C concentrations and activities are only transient and usually return to baseline levels seven days after treatment has been discontinued.
The most common side effects in patients treated with caplacizumab include bleeding events in various areas of the body (nose, gums, etc.) (7, 8, 9, 10). Due to this increased risk of bleeding in patients receiving caplacizumab therapy, concomitant treatment with platelet aggregation inhibitors, unfractionated or low molecular weight heparin, or oral anticoagulants requires a specific risk-benefit assessment and close clinical monitoring.
References
[1] Ulrichts H, Silence K, Schoolmeester A, et al. (2011): Antithrombotic drug candidate ALX-0081 shows superior preclinical efficacy and safety compared with currently marketed antiplatelet drugs. Blood; 118: 757–65.
[2] Callewaert F, Roodt J, Ulrichts H, et al. (2012): Evaluation of efficacy and safety of the anti-VWF Nanobody ALX-0681 in a preclinical baboon model of acquired thrombotic thrombocytopenic purpura. Blood; 120: 3603–10.
[3] Scully M, Hunt BJ, Benjamin S, et al. (2012): Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol; 158: 323–35.
[4] Sadler JE. (2008): Von Willebrand factor, ADAMTS13 and thrombotic thrombocytopenic purpura. Blood; 112: 11–8.
[5] Deford CC, Reese JA, Schwartz LH, et al. (2013): Multiple major morbidities and increased mortality during long-term follow-up after recovery from thrombotic thrombocytopenic purpura. Blood; 122: 2023–9.
[6] Hughes C, McEwan JR, Longair I, et al. (2009): Cardiac involvement in acute thrombotic thrombocytopenic purpura: association with troponin T and IgG antibodies to ADAMTS 13. J Thromb Haemost; 7: 529–36.
[7] Peyvandi F, et al. (2016): Caplacizumab for Acquired Thrombotic Thrombocytopenic Purpura. N Engl J Med; 374: 511–22.
[8] Scully M, et al. (2019): Caplacizumab Treatment for Acquired Thrombotic Thrombocytopenic Purpura. N Engl J Med; 380: 335–46.
[9] Peyvandi F, et al. (2021): Caplacizumab prevents refractoriness and mortality in acquired thrombotic thrombocytopenic purpura: integrated analysis. Blood adv; 5 (8): 2137–41.
[10] Mazepa MA, et al. (2019): How targeted therapy disrupts the treatment paradigm for acquired TTP: the risks, benefits, and unknowns. Blood; 134 (5): 415–20.